Diabetes is consistently a top three cost driver for pharmacy spend
Medications for diabetes and metabolic syndrome – also known as pre-diabetes – drive a large portion of pharmacy spend for most plan sponsors. Historically, achieving optimal medication adherence among diabetes patients has also been a challenge. Adherence is critical to ensuring better health outcomes and preventing costly and serious adverse events and complications.
(Source: RxBenefits Book of Business, 2023)
(Source: Economic Costs of Diabetes in the U.S. in 2022 | Diabetes Care | American Diabetes Association)
Pharmacist Led, Human to Human
Many programs focus on meter readings to drive outreach. The Tria Health approach focuses on proactively engaging members with a designated pharmacist as their personal advocate, providing disease education, care coordination, and support.

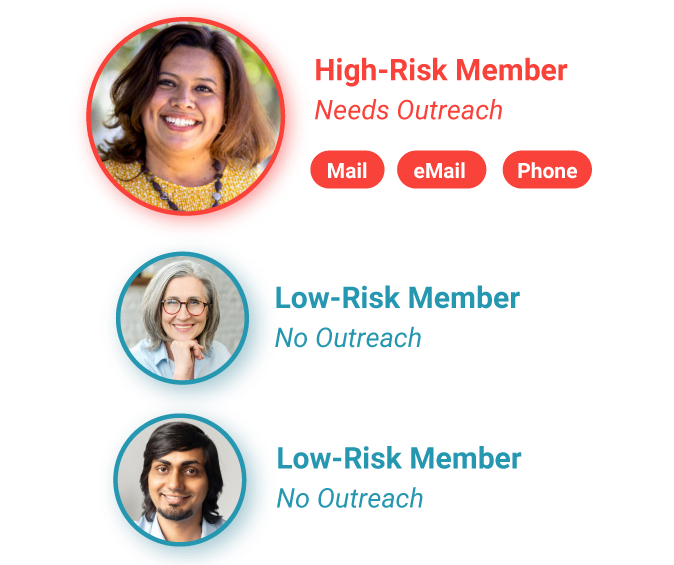
Proactive Outreach Improves Engagement
High-risk members are identified through pharmacy claims analysis on an ongoing basis. Once identified, members receive proactive outreach via mail, email, and phone to schedule a telephone appointment with a Tria Health pharmacist. An incentive is offered to members to encourage participation in the program. This multi-channel outreach maximizes engagement for these high-risk members.

Pharmacist Consultations Optimize Diabetes Management
Chronic conditions are managed with medications, making pharmacists the best resource to conduct confidential consultations with members. During each consultation, Tria Health’s pharmacists take the time to understand a patient’s background, behavior, and beliefs – all important factors in how they manage their health. By understanding a member’s motivations, along with a comprehensive medication and lifestyle review, Tria’s pharmacists work with members to develop a personalized care plan. Care plans are shared with the member’s primary care physician and other treating physicians and are used as the baseline for continuous management.
The results speak for themselves

For additional information, please contact your RxBenefits Account Team or Business Development Representative








