Is there a correlation between delayed diabetes diagnosis and the COVID-19 pandemic?
National Diabetes Awareness Month begins this November. According to the International Diabetes Federation (IDF), 34.2 million people in the US have diabetes. That accounts for 10.5% of the US population, which is one of the highest prevalences of diabetes in the world. More alarmingly, research by the Diabetes Research Institute published in 2020 showed that 7.3 million adults aged 18 years or older who met laboratory criteria for diabetes were not aware of or did not report having diabetes (undiagnosed diabetes). This number represents 2.8% of all US adults and 21.4% of all US adults with diabetes.
Pharmacist and clinical consultant, Brian Maas, recently reviewed Confidio pharmacy claims data to see if there was a correlation between delayed diabetes diagnosis and the COVID-19 pandemic.
Importance:
A recent survey by Diabetes UK, composed of almost 4,000 people living with diabetes, mirrors the bleak findings of the COVID-19 pandemic impact.
- One-third of people with diabetes had consultations canceled that have still not taken place
- One-third of people said they had not had contact with their diabetes team since the start of the pandemic
- 45% reported having difficulties managing their diabetes during the pandemic, most of whom referred to lack of access to care and support by their diabetes healthcare team as the reasons
In addition, a study based in Germany published in the Journal of the American Medical Association (JAMA) in July 2020 showed delayed care in new-onset type 1 diabetes. The study found a proportion of youth presenting with diabetic ketoacidosis (DKA) at diabetes diagnosis in Germany at 44.7%, nearly doubled from the same period in the 2 years prior, at 24.5% in 2019 and 24.1% in 2018. The study correlates COVID-19 obstacles delaying the presentation, or increasing the effort for a presentation, to the family doctor or in the clinic.
Pandemic New Utilizer Impact:
In reviewing book-of-business claims, we attempted to assess the number of new utilizers to diabetic therapy, with the expectation that there would be increased utilization driven by first-time members due to delayed diabetic diagnosis stemming from the pandemic.
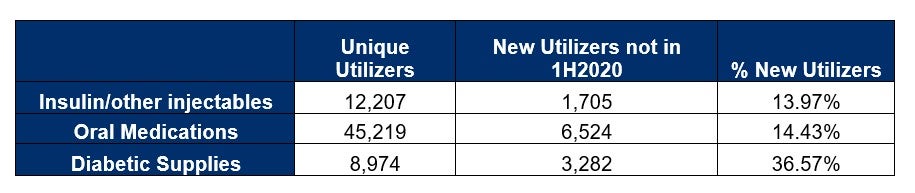
First, comparing 1H2020 to 2H2020, we captured increases in new utilizers across three key components of diabetes care. Lockdowns and social distancing began in March 2020, with some lifting of restrictions in late 4Q 2020. Thus, it made sense to see a nominal increase in new utilizers.
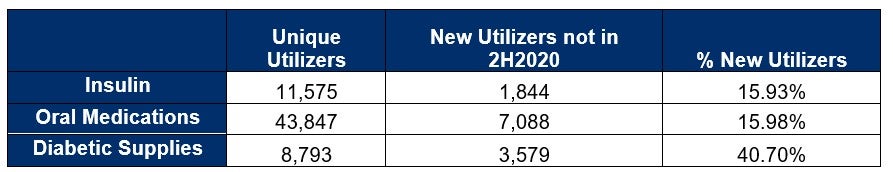
Comparing 2H2020 to 1H2021, we noted even more substantial growth for new utilizers as more pandemic related restrictions were lifted, and COVID-19 vaccinations took foothold. Thus, more people were going to visit their healthcare provider in person and obtaining the necessary lab values for a diabetic diagnosis.
Finally, comparing 1-3Q2020 to 1-3Q2021, we have a much more robust data set. We noted the trend of new utilizers across three key components of diabetes care continued to rise markedly across its book-of-business.
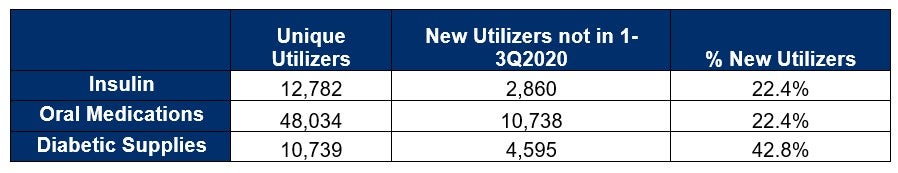
From the data above, it could be reasoned that the increase of new utilizers for diabetic management is in direct correlation to patients returning to the physician office for routine check-ups and scheduled labs.
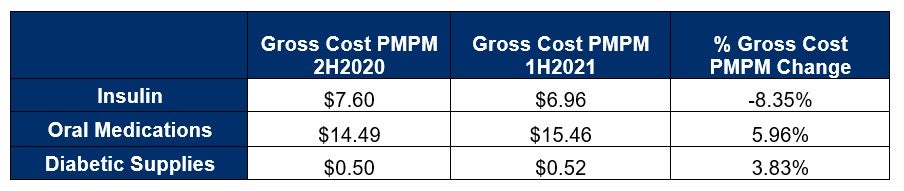
Pandemic New Gross Cost PMPM Impact:
From a Gross Cost PMPM perspective, comparing 1H2020 to 2H2020, we noted that the Diabetic Supplies category experienced the largest percent increase for Gross Cost PMPM. Some of this increase in diabetic supplies could be attributed to stockpiling during the early stages of the pandemic, similar to what was seen with store shelves being emptied of necessities such as toilet paper.
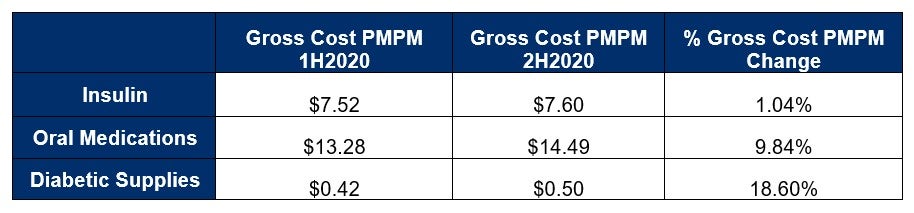
Comparing 2H2020 to 1H2021, we noted that the Insulin category experienced a nominal percent decrease for Gross Cost PMPM, while Oral Medications and Diabetic Supplies slowed in terms of rising Gross Cost PMPM. Here again, we could see previous stockpiling affecting the Gross Cost PMPM change. Members may have had ample supplies from the second half of 2020.
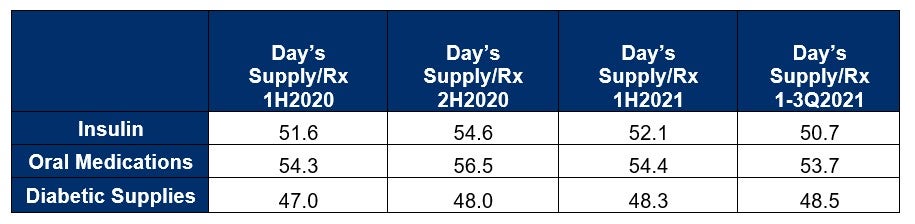
Pandemic Day’s Supply Impact:
Early in the pandemic, we noted the loosening of early refill restrictions by the PBMs, which allowed members to obtain 1-time early refills since the nation was on lock-down and members were concerned about having vital diabetic medication and supplies on hand. As result, we noted a Day’s Supply/Rx increase of 4% comparing 2H2020 to 1H2020 during the height of the pandemic. In 2021, we’ve seen days’ supply return to pre or early pandemic levels.
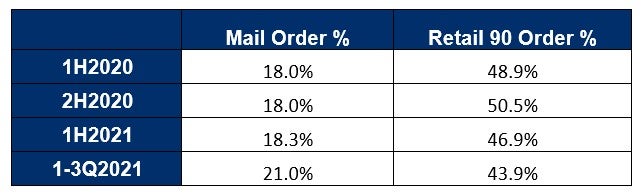
Pandemic Mail Order and Retail 90 Impact:
When assessing the impact to mail order and retail-90 claims, we need to recall that PBMs also encourage members to shift their retail-30 prescriptions to mail order or retail-90, to address safety concerns during periods of lockdown. This allowed members to obtain a three-month supply, without having to leave their home, or visit their pharmacy less frequently.
We did not note any substantial increases in terms of a shift to mail order during the early periods of the COVID-19 pandemic. However, there was a 4.55% shift to retail-90 in the second half of 2020 as compared to the first half of 2020, as PBMs were encouraging 90-day supplies for diabetic maintenance medications.
Summary:
It is likely that you have seen the diabetes class affect plan costs since the start of the pandemic. While many plans have seen an increase in pharmacy costs associated with the treatment of diabetes, the true extent of total diabetes health care costs associated with the pandemic have yet to be fully realized. Recent publications have reported how significantly the pandemic has impacted the diabetic population; from an increased risk of complications associated with diabetic ulcers to an increase of ICU admissions from patients delaying necessary care including prescriptions and medical visits. When fully realized the secondary health care costs will likely be far more impactful than the increase in pharmacy spend for many plans. Results, such as the data presented above, draw awareness to the diverse and pressing care gaps caused by the COVID-19 pandemic and reconfirms the importance of early and ongoing access to care. We feel steps, such as telemedicine, can provide a roadmap for necessary remedial action that ensures undisrupted diabetes management. A proactive, holistic approach will be required to get patients back on track.
While telemedicine can work, face-to-face consultation works better to encourage people to manage their diabetic condition themselves and change the habits of a lifetime.





